Medical-Related PTSD Part Two: Special Needs Caregiver Trauma
Note: I may earn money or products from the companies, products, or links mentioned in this post.
Diagnosed With Medical PTSD and now Sharing my Story to Raise Awareness
Ever since I was diagnosed with medical-related PTSD, I’ve been afraid to tell my story. I’ve been afraid of people’s thoughts and knew that a lot of people would have a hard time understanding.
In the military community, PTSD is a very serious thing. Since I partly write a military blog, I wasn’t sure how my writing about this topic would be taken. I definitely don’t want my topic to shadow the importance of combat-related PTSD and the public’s knowledge and awareness of it.
On the other hand, medical-related PTSD is very real and very unknown to the public. I knew I had to share my story so that I could bring anybody awareness and hopefully to help others who may have gone through the same thing. This is a very tough topic for me and it’s been very hard, but also cathartic for me to write about.
The first part of this story was birth trauma during my son’s birth. If you missed that part be sure and go back and read it first. That birth trauma was just a small part of the entire story that led to me being diagnosed with medical-related PTSD earlier this year. This is the second part of my story.
Special Needs Caregiver Trauma: Autism
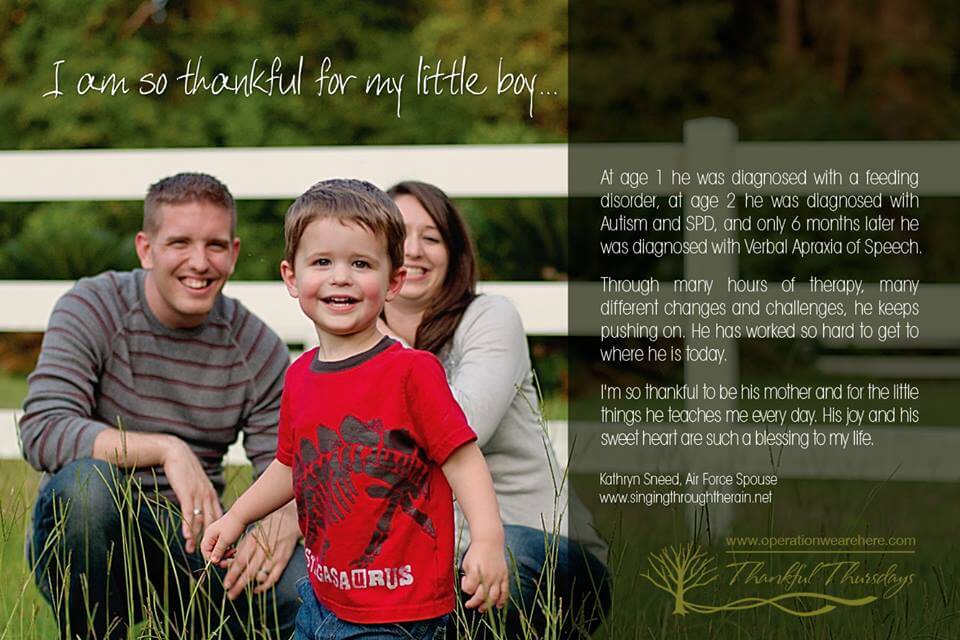
The anxiety that came with the birth of my son only continued to grow as he got older. He’d had problems since birth that no doctor would acknowledge, but things had gotten worse during my husband’s deployment. During that time we were told that my son most likely had autism.
While we were waiting on a diagnosis, many other medical tests were done to rule things out. My son also ended up in the hospital during this time. He had been very sick for weeks and was dehydrated. One Sunday night we ended up in the emergency room. He needed IV fluids, but it wasn’t as easy as that. He wasn’t going to let anyone touch him.
They told me they would have to wrap him up in a sheet so that he couldn’t fight as much. This would help them get the IV in. Because he was so dehydrated, it took more then 30 minutes to get the IV in. Two nurses worked on getting the IV in his arm, my friend was helping hold his upper body still, and I was holding down his still-kicking legs. Inspite of our efforts he continued to fight, scream, and cry. It was awful as I held him down and tried to keep the tears that I too had from falling.
As he continued to need more medical tests, it only got worse. It always started with three or four doctors and nurses trying to keep him calm, and me helpless to do anything to make it better. For one of these tests they needed to put him under. We were allowed to stay in the room during this time, but I wish we hadn’t been.
They gave him the medicine and he should have been asleep, but he was still fighting. Screaming. Crying. Needing me, his mom. The doctor told the nurse he needed more medicine to put him to sleep, and at that point I couldn’t stay and watch anymore, I left the room in tears.
Things got a little better as my son got older. He had been officially diagnosed with autism and was in all kind of therapies and interventions. The stress was hard though as we had a rigorous schedule, and the ups and downs of therapists coming and going left me in tears more often then naught.
By this point, I realized I needed to be on medicine for anxiety. I had been in counseling for awhile and we had talked about the help the medicine would bring. It was a welcome reprieve.
Years later as the things got better with my son, we decided to have another baby. We knew that there was a chance that baby could also have autism, but we never imagined the medical complexities we would face with our second child.
Special Needs Caregiver Trauma: Medical Complexities
Soon after my daughter was born we discovered she had severe reflux. Projectile vomiting was a common occurrence every day and so was choking during her bottle feedings. By the time she was two months old, we discovered things were much worse then we thought. She had several tests and we heard words like Failure to Thrive, Laryngomalacia, and Aspiration.
We were told that she wasn’t gaining weight, that when she was being fed she was aspirating on her food (going into her lungs) and causing her to choke. Because she had severe reflux she was also aspirating on the reflux that was coming back up. Multiple times a day she was choking and there was nothing we could do, but make sure she was propped up.
Soon she was admitted to the hospital. More testing, a feeding tube through the nose, and wires everywhere. We were sent home after a week, but we didn’t even make it 24 hours before she was admitted again, this time for surgery. They did two surgeries at the same time, a Fundoplication and a feeding tube that was inserted into the stomach. Letting my three month old baby go with those doctors for surgery was the hardest thing I’ve ever done.
Only two weeks after we got home from the hospital, she was admitted again, this time in Atlanta. She had been having what seemed like choking spells every day since we left the hospital. It all came to a head when she started turning beet red and looked like she couldn’t breathe.
By this point my nerves were shot. During one of the hospital stays I had called my doctor and told her I needed to go up on my anxiety medicine. I knew I wasn’t handling things well and I needed help. I was barely sleeping for fear she would choke and die in her sleep. Every cough, every weird breath had me running in to check on her during the night, multiple times a night.
We spent two weeks in the hospital in Atlanta. They ran every test the doctors could think of and even some that I thought of. After two weeks of testing the only thing they were able to find was central and obstructive apnea. Other than that, they weren’t sure why she was having these “choking” episodes or why she was struggling to gain weight even with the feeding tube.
The hospital has us take a CPR class to learn what to do for the choking episodes and then sent us on our way. They told us there was not much we could and that as long she wasn’t turning blue she was fine. But the episodes continued up to 20 times a day.
As the months went on, things got worse and finally we decided to go to Boston to get more testing and another medical opinion. Hospital stay after hospital stay came and went. Different hospitals every time. Sometimes it was because she was so sick, other times it was for IV antibiotics. By the end of the year, she had been hospitalized a total of 7 times not including emergency room visits, and had spent over 7 weeks total in the hospital.
As more tests came and went, I began to grow numb. The doctors and nurses would tell me they were surprised I wasn’t crying and they didn’t know how I was so calm. I didn’t have time to cry, I had to be strong for my baby. I wasn’t calm, on the inside the storm was raging and the numbness just grew.
The anxiety was severe. Any sign of sickness in my kids sent me into a panic attack for thought of something serious and having to stay in the hospital again. The obsession with finding answers had grown. I spent hours and hours on the internet searching for answers. Something, anything that would explain what was going on with my daughter.
Although the choking episodes had gotten better and were almost non-existent, coughing or choking of any kind in child or adult, would send me into a panic. It was like being slammed in the face with everything we had been through with my daughter.
A friend’s child would choke a little on her food, and I would freak out. On the inside it was even worse. I would wonder why no one was doing anything, why everyone was so calm. A child was choking. But when I came out of the haze, I looked around I realized that what I had thought was choking was just a little cough to clear the food or just a little water going down the wrong pipe.
I would have flashbacks watching shows that had a child in the hospital or going into surgery, and I would have to change the show before I had a full blown panic attack. I would have nightmares about people choking. Just choking over and over and nothing could stop it.
Almost nightly I was having panic attacks and unable to sleep. The sleep medicines the doctors gave me did nothing to help. I started having chest pains and several times I almost went to the hospital thinking I was having a heart attack. I finally realized I needed help and went to see my doctor who again upped my anxiety medicine.
Finally, I mentioned to my counselor what was going on. She told me that what I was experiencing was symptoms of PTSD. In a way, I wasn’t surprised. I knew this was more severe then a little anxiety.
Everything came to a head when we received three month’s notice that we were moving across the country. We still had not found answers, I still had two kids in therapy and a daughter who was at the time seeing 6 different specialists. The stress was enormous.
The week before the movers came, I literally started losing it. The stress of moving plus dealing with several infections in my daughter that were not responding to antibiotics. I felt like I was having a breakdown, I was having severe panic attacks and it was so bad that I almost took myself to the hospital to ask for help and relief.
I finally ended up at the doctor’s office, sitting in the chair shaking uncontrollably from the anxiety I was feeling. The doctor decided to put me on something a different. It was a lot stronger then anything I had taken before and I’m still on it today. It’s helped more than I can say, and I am thankful that I was able to re-gain some control.
Before we moved. My counselor told me to seek out someone here that knew how to do EMDR therapy. I’m happy to say that I have found a good Christian counselor who is trained in EMDR and she wants to start the therapy with me this summer. I’m excited to see how it’s going to help and how hopefully it will change my life.
I share my story to raise awareness. Combat-related PTSD it not the only type of PTSD that exists. Caregiver trauma and PTSD due to caring for children that have special needs is real.
~ ~ ~
“Mothers of adolescents and adults with autism experience chronic stress comparable to combat soldiers and struggle with frequent fatigue and work interruptions, new research finds. These moms also spend significantly more time caregiving than moms of those without disabilities.” – Autism Moms Have Stress Similar to Combat Soldiers
~ ~ ~
“Over dinner we talked about how we both feel like crazy people lately, and I shared with him my theory that all special needs parents have my newly created diagnosis: CTSD (continued traumatic stress disorder).
How else do we make sense of this extremely volatile reaction we’re both having to Julia starting a new medication. We’ve been complete basket cases this past month prepping for and starting these steroids.
Because we’re traumatized.
Because this past month isn’t just about one new med; it’s the culmination of seven years of unresolved trauma. Seven years of stuffing grief and swallowing fear to keep functioning one day at a time for the girl we love.” – A New Diagnosis All Parents of Special Needs Children Will Understand
~ ~ ~
Special Needs Parents and PTSD Series From Different Dream:







OK. I will admit this…I had to get tuned to be able to read your story, and I have one of the most severe cases of combat trauma you will ever hope not to see. I am homebound…to keep the rest of the world safe.
PTSD is what it is, regardless of the cause. There is no preferred frame of reference. I got it from doing things that allow no forgiveness, only atonement….but that is ONLY a category, and never, never a comparison of virtue or vice.
Damn it, I am crying too hard to write more. I just wish you my very very very best.
You have such a gift of your writing. I cried since I could so relate with so many of your words. Thank you for sharing your gift.
As a mom, I was crying as I read all the struggles you went through with your children’s health. My daughter had some reflux but nothing like that. I can imagine how traumatizing that and the issues with your son were. My husband suffers from PTSD. The source doesn’t lessen its impact on you. I am glad that you have found a good counselor. I wish you well on your journey.
Traci
Kathryn, what an amazing heartfelt and honest post! thank you for sharing. I will pray for you and your family. May God bless you and your little ones too
What an amazing story traveling through your PTSD. I can’t begin to explain what your story meant to me as I was reading it. I wish I could put into words how I feel and what I’ve gone through in my life as well as you have done so here. You walked through the fear of others knowing and have helped others, and myself, realize that it’s Ok…that it’s ok, to feel! Thank you so very much for sharing.
Thank you for writing your story. My 8 year old son has faced a life time of medical issues. More surgeries than I can count. I face absolute fear when we have to see a new specialist. Will they understand? Will they be able to help or just send us on our merry way?
I am a medical professional and never understood what life from this side of the bed entailed. I would look at the parents of my patients and could tell they looked shell-shocked but still had no idea what they were truly feeling. That was until I made my own journey to the other side of the bed as a parent of a chronically ill child. I see now, first hand, the trauma they endure. To watch your child go through unrelenting pain with help seeming impossible is traumatic in itself. To have to fight for a diagnosis is traumatic. To have to realize that a cure isn’t going to happen is traumatic. Never knowing when your child may end up in the hospital again is traumatic. Never knowing how long the stay will be is traumatic. Every new med, praying it works. Every new specialist, will they have answers. Every new procedure, what am I putting my child through. The questions never end. The searching never ends.
I’m considering pursuing my doctorate for the sole reason that I want to research this topic more. I want this to be the focus of my doctoral research. We have to develop more ways to identify and help PTSD in the parents of chronically ill children.
Thank you!
Your story sounds so much like mine and the stories of many, many parents of kids with major medical special needs. Thank you so much for the links to the DifferentDream.com series and for adding this to the website’s Tuesday special needs link share.
Thanks Jolene. It was reading your series that made me brave enough to share! So glad I am not alone in this.
Thank you for sharing your story. I didn’t know very much about caregiver PTSD and your experience is very insightful. I have done some EMDR with my therapist and found it to be really helpful. Good luck!
Kathryn,
I am so, so glad you put this out there. There needs to be so, so much more awareness and understanding of PTSD. This last year, I went through some similar issues – we also used EMDR for me and it worked extremely well. Glad you found something that worked…. Thank you again for posting this.
Charity
(remember, I used to be in contact with you like SIX years ago – I’m from Her Price is Far Above Rubies – which is now discontinued but anyway… 🙂 Good to start reading you again.)
thank you for sharing…. I can relate to SO much of it… SO much of it, traumatic deliveries, autism, child struggling to breathe and more… I’m trying to hard to understand and cope with everything…
I’m so sorry. Have you tried counseling? It can help so much! Prayers for you and I hope that you can find healing.